In a move that signals a proceeded advancement in how the American healthcare framework measures and incentivizes high-quality quiet care, five noticeable healthcare quality pioneers have tended to a proposition for a modern benchmark centering on post-acute care release rates, especially the rate of release to post-acute care offices versus domestic. This consideration reflects a developing industry acknowledgment that conventional quality measurements, whereas crucial, may not completely capture the all encompassing productivity, community integration, and patient-centricity of present day healing center services.
Background and Authentic Setting: The Walk for Quality
The thrust to measure and make strides healthcare quality is not unused; its roots follow back to the mid-19th century with pioneers like Florence Songbird and the early 20th century with specialist Ernest Codman, who championed following understanding results by means of “Conclusion Result Cards.” The formal quality development picked up noteworthy energy in the last mentioned half of the 20th century, strikingly with the foundation of Medicare and Medicaid in 1965, which presented government supervision and set the foundational “Conditions of Support” for hospitals.
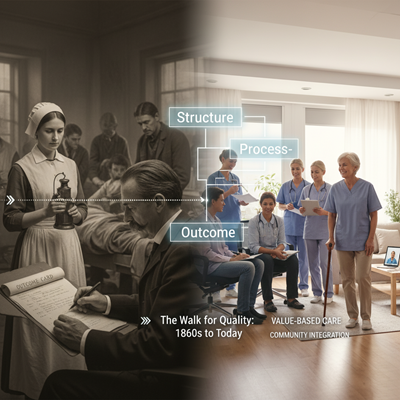
A essential minute was the work of Avedis Donabedian in the 1960s, who formalized the Structure-Process-Outcome demonstrate, which remains the spine of quality measurement:
- Structure: The setting in which care is conveyed (e.g., office, staffing ratio).
- Process: The particular activities taken to convey care (e.g., taking after clinical guidelines).
- Outcome: The comes about of the care on the patient’s wellbeing (e.g., mortality, readmission).
More as of late, the move toward value-based care—incentivizing quality over quantity—has intensified the significance of measurements. Activities like the Centers for Medicare & Medicaid Services’ (CMS) Healing center Readmission Diminishment Program have tied monetary punishments to measures like 30-day readmission rates. The unused center on post-acute release rates is a coherent another step in this advancement, moving past exclusively clinical measurements to join broader concepts of care coordination and understanding readiness for life after the intense healing center stay.
The Current Slant: Post-Acute Release as a Quality Proxy
The particular benchmark beneath consideration—measuring the rate of release to post-acute care offices (such as gifted nursing offices or recovery centers) versus release straightforwardly to the patient’s home—stems from inquire about highlighting the significant variety in these rates among U.S. hospitals.

Experts contend that a tall rate of release to post-acute care, indeed when risk-adjusted, can in some cases be a intermediary for:
- Gaps in Care Coordination: The clinic may be falling flat to orchestrate satisfactory home-based assets (like domestic wellbeing or tough restorative hardware) or to include community partners.
- Increased Fetched and Chance: Post-acute care settings are ordinarily more costly than domestic care and are frequently related with higher rates of readmission and mortality.
Consequently, pioneers see a tall, risk-adjusted ‘discharge to home’ rate as a marker of all encompassing, effective, and inventive care conveyance that ranges the whole continuum, emphasizing quiet strengthening and community health.
Expert Suppositions: Adjusting Quality and Safety
The five pioneers who weighed in on the proposition recognized the measure’s potential whereas focusing basic caveats:
- The Control of Hazard Adjustment
Experts generally concurred that the degree must be thoroughly risk-adjusted. As one Chief Quality Officer famous, without altering for the sort of major surgery, quiet comorbidities, and social determinants of wellbeing (SDOH), the metric might unjustifiably penalize clinics serving more wiped out or more socioeconomically distraught populaces. Hazard alteration is fundamental to guarantee a reasonable comparison of clinic performance.
- The ‘Home is Best’ Reasoning and SDOH
The reasoning of “Domestic is Best” drives the degree, but its possibility is significantly affected by Social Determinants of Wellbeing (SDOH). Variables like progression of care, family back, lodging solidness, and get to to transportation play a vital part in deciding the most fitting and most secure release area. A quality pioneer from a framework serving country populaces highlighted the need of wellbeing system-community organizations to create the essential domestic wellbeing assets, expressing that release rates are a great intermediary for an organization’s “all encompassing considering” approximately care conveyance over the continuum.
- The Hazard of Risky Discharges
A noteworthy concern raised is the potential for this metric, created with the best of eagerly, to accidentally weight care groups into making risky releases. A Bad habit President and Chief Quality Officer commented that no single metric can accomplish each objective and that a particular center on the rate seem lead to patients being sent domestic rashly if satisfactory post-discharge care courses of action haven’t been secured, possibly expanding the hazard of readmission or complication. This underscores the require for multi-faceted estimation and near observing of results over time.
Implications for the Healthcare System
The appropriation of this benchmark would have wide implications:
Focus on the Continuum of Care
Hospitals would be incentivized to grow their center past the four dividers of the intense office. This move would require more prominent speculation in:
- Care Coordination: Strong release arranging, follow-up calls, and understanding education.
- Community Associations: Collaborating with domestic wellbeing offices, social administrations, and community-based organizations to fill asset holes, especially those related to SDOH.
Incentivizing Proficiency and Innovation
By fulfilling secure release to domestic, the degree verifiably advances more noteworthy effectiveness inside the intense care setting, decreasing possibly superfluous longer lengths of remain utilized to orchestrate care. It too goads development in creating low-cost, high-impact procedures like prehabilitation for surgical patients and strong hazard appraisal devices to direct disposition.
Transparency and Open Accountability
Incorporating this metric into open announcing, nearby existing measures like readmission rates and mortality, would improve straightforwardness. It gives shoppers and payers a more comprehensive picture of a hospital’s execution in overseeing the whole scene of care—from confirmation to fruitful recuperation at home.
The discussion among these five pioneers makes it clear that the following wilderness of healing center quality estimation requests a metric that is not as it were clinically sound but moreover socially educated, viably measuring a hospital’s capacity to provide not fair an great method, but an fabulous recuperation.





