A key challenge confronting advanced healthcare frameworks is overseeing the stream of patients—from confirmation to discharge—efficiently and securely, particularly in the midst of rising request and sharpness. The Penn Pharmaceutical wellbeing framework, a huge scholarly restorative center enveloping seven acute-care healing centers, has handled this issue head-on with a centralized, system-wide capacity administration demonstrate. This activity is demonstrating effective in optimizing asset utilization, moving forward quiet get to, and guaranteeing that specialized care is accessible for the most debilitated patients.
Background and Chronicled Setting: The Need for Centralization
Historically, persistent stream and capacity administration in expansive, multi-hospital frameworks like Penn Pharmaceutical were frequently decentralized, working on a departmental or person healing center premise. This siloed approach driven to wasteful aspects, such as uneven dispersion of patients, expanded hold up times in Crisis Offices (EDs), and troubles in rapidly exchanging patients who required exceedingly specialized administrations as it were accessible at one facility.
The need for a more cohesive procedure got to be especially intense due to a few long-term patterns and outside shocks:
- Rising Persistent Sharpness and Volume: As a major scholastic center and transplant center, Penn Medication reliably oversees a tall volume of complex, high-acuity cases.
- The COVID-19 Widespread: The widespread uncovered the delicacy of decentralized capacity arranging, underscoring the require for a bound together command structure to oversee surge capacity, staffing, and asset allotment (like ventilators and PPE) over the whole system.
- National Capacity Weight: Wellbeing frameworks across the nation confront expanding request that regularly surpasses the accessible beds, making productive persistent throughput a basic metric for quality and money related stability.
In reaction to these weights, Penn Medication propelled a critical capacity administration activity, centralizing already dissimilar functions.
The Current Show: A Centralized Center for Quiet Flow
Penn Medicine’s capacity administration demonstrate is on a very basic level a move toward system-wide bed administration and coordination. As of mid-2025, the exertion has extended into a bound together capacity administration center that coordinating a few basic services:
- Centralized Bed Administration: Supervising the assignment of inpatient beds over all three Philadelphia-based healing centers (counting the Healing center of the College of Pennsylvania, a major transplant center) and planning stream over its seven acute-care facilities.
- Transfer Center Integration: The capacity center encourages both inner patient transfer (between Penn Pharmaceutical clinics) and outside transfer (from exterior healing centers, now and then from around the world). In a later financial year, the center overseen over 9,200 understanding transfers.
- Emergency Transportation Administrations: The PennSTAR flight program and the PennComm flight alacrity center are coordinates into the center, guaranteeing quick, facilitated transport for fundamentally sick patients.

This centralized structure is outlined to coordinate the system’s “supply” (beds, staff, specialized hardware) with “request” (inbound patients) in real-time, moving absent from the ancient attitude of ‘If they arrive in your building, they’re yours’ to a system-wide see of resources.
Focus on Length of Remain (LOS)
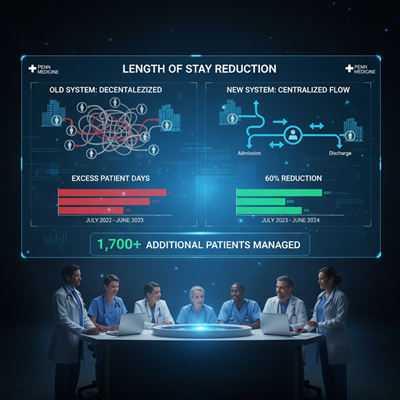
A vital component of the demonstrate is an inside exertion to decrease abundance understanding days—the additional days a quiet remains hospitalized past what is ideal for their condition. By effectively tending to the bottlenecks that delay release (such as post-acute care situation or last doctor sign-offs), the framework accomplished a generally 60% diminish in overabundance quiet days in one monetary year (July 2023 to June 2024). This effectiveness pick up permitted the framework to suit an assessed 1,700 extra patients without including unused physical beds.
Expert Conclusions and Current Patterns: Operations Administration in Healthcare
Experts in operations administration and healthcare organization see this centralization as a fundamental evolution.
Dr. Robin Wood, Bad habit President for Framework Capacity and Persistent Stream at Penn Medication, has underscored the move in considering: “To have the capacity for the most debilitated of the debilitated, we require to make beyond any doubt our supply is coordinating our demand.” This reflects a developing slant over driving U.S. wellbeing frameworks to embrace a “command center” approach, which utilizes real-time information analytics, advanced operational arranging, and centralization to optimize persistent flow.
In the broader healthcare industry, capacity administration is progressively moving past basically following open beds:
- Leveraging Innovation: The worldwide showcase for clinic capacity administration arrangements is encountering quick development, driven by the integration of Artificial Intelligence (AI) and machine learning for prescient analytics. These apparatuses offer assistance estimate understanding confirmations and release designs, empowering proactive asset allocation.
- Focus on Quiet Stream and Coordinations: Present day models emphasize optimizing the whole persistent travel, counting transport coordinations and opportune turnover of rooms by natural administrations staff. Cases classified as “Level 0” crises, for illustration, have a objective of exchange into a Penn office inside two hours, requesting an quick, coordinated group response.
- Hospital-at-Home Models: Whereas Penn Medicine’s capacity center centers on inpatient stream, the broader drift of Hospital-at-Home (H&H) programs, which Penn Pharmaceutical has moreover investigated, speaks to a procedure to decrease the physical bed request by conveying acute-level care in the patient’s home.
Implications: Get to, Quality, and Monetary Health
The fruitful usage of Penn Medicine’s capacity administration demonstrate has noteworthy suggestions for patients, clinicians, and the wellbeing system’s sustainability.
Improved Understanding Get to and Quality
By diminishing overabundance days and streamlining exchanges, the framework can more reliably “make space for wonders,” as one inner report portrayed it. This means:
- Faster Get to to Specialized Care: Basically sick patients requiring life back (like ECMO), injury, or specialized neurosurgery can be exchanged and conceded speedier, which is specifically connected to way better persistent outcomes.
- Reduced ED Boarding: Proficient throughput is fundamental for decreasing the sum of time patients hold up in the crisis division for an inpatient bed—a common metric of clinic packing and a hazard to quiet safety.
Operational and Monetary Efficiency

The operational picks up interpret straightforwardly into budgetary benefits. The capacity to care for thousands of extra patients without building unused foundation illustrates the system’s upgraded money related resiliency. Tall utilization, when overseen successfully with moo hold up times, maximizes both persistent benefit and revenue.
Shifting Organizational Culture
The show requires a social move toward framework considering. It requires intrigue collaboration, straightforwardness of assets over all clinics, and responsibility to a central, data-driven operational arrange. This solidarity of reason is key to exploring the complex, high-stakes environment of a major scholarly restorative center. The centralized capacity center, in this manner, acts as the nerve center for clinical decision-making and convenient asset administration, guaranteeing that both common medicines and exceedingly specialized intercessions can be conveyed when and where they are required most.





