The advanced healthcare scene is a complex embroidered artwork of high-stakes clinical choices, perplexing money related administration, and advancing administrative requests. At the heart of this framework is a lasting challenge: bridging the gap between authoritative and clinical groups. This division, frequently characterized by varying priorities—patient care versus cost-efficiency—can lead to communication breakdowns, wasteful aspects, and, fundamentally, problematic persistent results. In any case, a developing development toward genuine integration is reshaping healing centers and clinics, seeing this relationship not as a struggle, but as a energetic association basic for conveying value-based care.
Background and Verifiable Context
The basic isolate between the “trade” and “restorative” sides of healthcare has profound chronicled roots. In the early to mid-20th century, numerous healing center chairmen were non-physicians, frequently medical caretakers, individuals of the clergy, or laypersons, whereas doctors worked with noteworthy independence. The rise of advanced innovation, complex protections frameworks, and expanded administrative oversight—particularly in the last mentioned half of the century—ushered in a modern time of professionalized healthcare management.
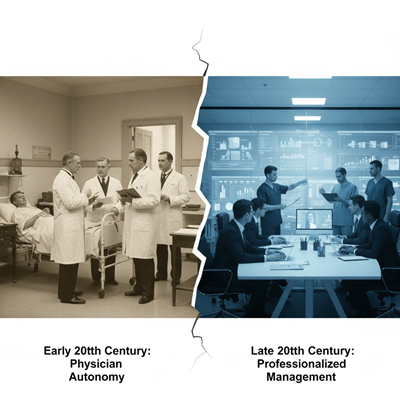
This professionalization, whereas vital for overseeing swelling costs and complexity, accidentally extended the gap. Chairmen, driven by monetary reasonability, asset assignment, and administrative compliance, started to be seen by clinicians as prioritizing the foot line over the bedside. Alternately, directors frequently see clinicians as being separated from the monetary substances of the organization or as abusing assets. This essential contrast in seen center values—profit-oriented versus patient-oriented—has verifiably come about in hostility and organizational silos, affecting everything from supply chain administration to electronic wellbeing record (EHR) implementation.
Current Patterns: A Thrust for Clinical Integration
Today’s healthcare environment, especially the worldwide move toward value-based care (VBC) models, is driving directors and clinicians to stand up to this separate. VBC, which incentivizes quality results and cost-efficiency over the volume of administrations (fee-for-service), cannot be accomplished without honest to goodness collaboration.\

Key patterns driving integration include:
- Digital Change: The far reaching appropriation of Electronic Health Records (EHRs), telemedicine, and wellbeing data administration (HIM) frameworks requires a combined exertion. Regulatory plan of EHRs that fall flat to meet clinical workflow needs can lead to doctor burnout and documentation mistakes. Coordination clinical input into innovation plan is presently a basic trend.
- Interoperability and Data-Driven Choices: The thrust for consistent information trade over distinctive frameworks and offices requires authoritative framework to back clinical information needs. Both groups must concur on standardized information sets and quality measurements, utilizing Enormous Information analytics to illuminate both clinical conventions and operational strategies.
- Collaborative Care Models: Clinical Integration Networks (CINs) and Accountable Care Organizations (ACOs) are formal structures that legally adjust clinics and doctors to move forward quality and diminish costs. These models intrinsically command interdependency, participation, and shared money related chance, in this manner driving integration.
Expert Suppositions: Shared Vision and Common Respect
Experts reliably point to a few center methodologies for fruitful integration, all centered on a principal move in organizational culture:

- Establishing a Shared Vision: “The objective of a clinic director is to make a positive work environment where patients are treated in the most proficient and cost-effective way conceivable,” notes one master examination. This principal, patient-centric mission must be expressly and together claimed by both sides.
- Open Communication and Straightforwardness: Customary, organized gatherings where clinical staff feel valued and heard are significant. Straightforwardness from organization on the method of reasoning behind major decisions—especially those affecting assets, staffing, or policy—builds believe. Doctors, in specific, ought to be included in discussions at the key and money related arranging levels, moving them from simply buyers of assets to active partners in asset management.
- Cross-Functional Preparing and Authority: Giving authority and team-building preparing for both regulatory and clinical pioneers makes a difference them get it each other’s “dialect” and needs. Regulatory preparing for clinical staff, and clinical introduction for regulatory staff, cultivates shared regard and compassion for their unmistakable, but forbid, challenges.
Dr. John Doe, CEO of an coordinates health system, frequently comments, “The clinician sees the prompt quiet, the chairman sees the populace. Both points of view are half-truths until they are brought together. Our best choices are continuously made at a table where a specialist, a nurture, and a monetary officer sit side-by-side.”
Implications for Superior Healthcare Outcomes
The results of the verifiable administrative-clinical isolate are extreme: expanded restorative mistakes, destitute asset assignment, doctor and staff burnout, and, eventually, compromised quiet security. The Joint Commission has reliably cited communication failures as a driving root cause for unfavorable clinical events.
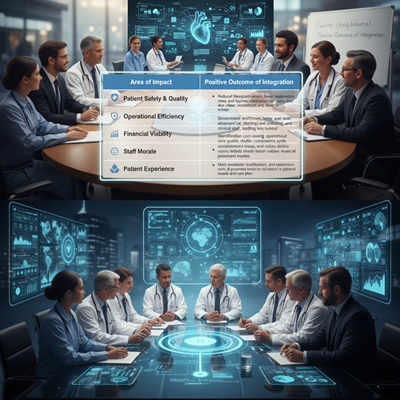
Then again, fruitful integration yields noteworthy positive implications:
| Area of Impact | Positive Outcome of Integration |
| Patient Security & Quality | Reduced therapeutic blunders, lower readmission rates, and progressed demonstrative exactness due to clear, standardized, and convenient data exchange. |
| Operational Efficiency | Streamlined workflows, way better asset allotment (e.g., staffing and planning), and decreased regulatory burden on clinical staff, driving to less burnout. |
| Financial Viability | Identification of cost-saving openings without compromising care quality, made strides income cycle administration, and victory beneath value-based installment models. |
| Staff Morale | Increased work fulfillment and a more grounded culture of cooperation, as clinicians feel their ability is esteemed in organizational strategy. |
| Patient Experience | More personalized, facilitated, and ceaseless care, as all group individuals are adjusted on the patient’s needs and care plan. |
In conclusion, bridging the hole between organization and clinical groups is no longer a matter of organizational preference—it is a vital basic for survival and victory in present day healthcare. The future of high-quality, cost-effective, patient-centered care rests on the capacity of these two sides to rise above their chronicled contrasts and co-create a really coordinates wellbeing framework.